Looking to modernize your Hospital, Lab or Clinic?
Hospi is trusted across 25 Indian states for billing, EMR, lab reports, automations & more.
Introduction
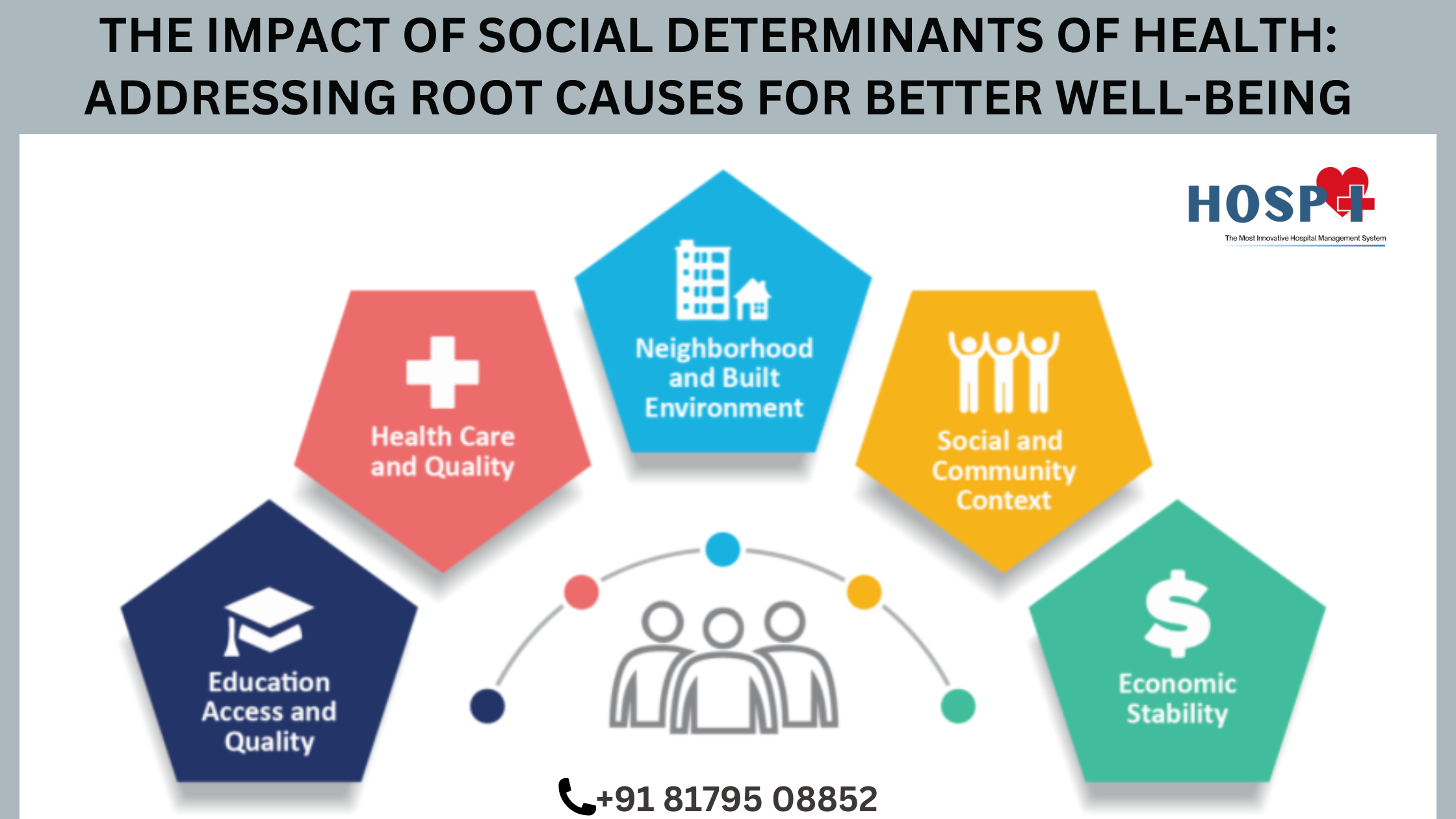
Healthcare extends far beyond hospitals, medicines, and clinical interventions. The social determinants of health (SDOH) play a defining role in shaping individual and community well-being. These determinants include economic stability, education, social environments, healthcare access, and physical surroundings. Addressing them is essential for reducing health disparities and improving outcomes at a systemic level.
In this comprehensive analysis, we will explore the impact of social determinants, analyze global case studies, and discuss actionable strategies to mitigate their effects on healthcare systems worldwide.
1. Economic Stability and Its Impact on Health
Economic stability determines an individual’s ability to access basic needs such as nutritious food, safe housing, and medical care. Financial insecurity increases the risk of chronic illnesses and mental health disorders.
Key Factors:
- Employment Opportunities: Higher-paying, stable jobs lead to better healthcare access.
- Poverty and Health Risks: Individuals in low-income brackets experience higher rates of obesity, diabetes, cardiovascular diseases, and depression.
- Housing Stability: Unstable housing conditions lead to increased stress, exposure to environmental hazards, and limited healthcare access.
Global Perspective:
- In Scandinavian countries, government-funded healthcare and universal basic income initiatives have significantly improved public health indicators.
- In contrast, the United States faces higher health disparities due to economic inequalities in insurance coverage and access to care.
Solutions:
- Expanding minimum wage policies and employment training programs.
- Enhancing housing assistance to ensure safe and stable living conditions.
- Strengthening financial support for low-income families to reduce health-related economic stress.
2. Education and Health Literacy: A Lifelong Impact
Higher education levels correlate with healthier lifestyles, informed medical decisions, and lower rates of chronic diseases.
Why Education Matters:
- Health Literacy: Educated individuals better understand medical instructions, disease prevention, and treatment adherence.
- Employment Link: Higher education leads to well-paying jobs that offer health benefits.
- Early Childhood Education: Programs like Head Start in the U.S. show that investing in early education leads to better lifelong health outcomes.
Global Insights:
- Countries like Finland prioritize education, leading to improved population health and longevity.
- India faces disparities in rural education, impacting healthcare literacy and maternal health.
Recommendations:
- Strengthen health education in schools.
- Promote lifelong learning programs to enhance public health knowledge.
- Expand vocational training to provide stable employment and healthcare benefits.
3. Social Support Networks: The Hidden Health Booster
A strong social network enhances mental and physical well-being, reducing risks associated with stress, depression, and chronic diseases.
The Role of Social Connections:
- Emotional Support: Strong family and community ties reduce anxiety and depression.
- Social Engagement: Involvement in community activities promotes mental resilience.
- Impact on Aging: Studies show that elderly individuals with active social lives experience lower rates of dementia and physical decline.
Case Studies:
- Blue Zones: In regions like Okinawa (Japan) and Sardinia (Italy), close-knit communities contribute to longevity and well-being.
- Urban Planning in Denmark: Designing cities with social engagement spaces fosters stronger community connections.
Actionable Steps:
- Encourage community-based health programs.
- Reduce social isolation among the elderly by implementing structured engagement initiatives.
- Support mental health programs that strengthen family and peer networks.
4. Healthcare Access: Bridging the Gap
Universal healthcare access ensures preventive care, early diagnosis, and effective treatment, reducing long-term healthcare costs and improving quality of life.
Barriers to Access:
- Lack of Health Insurance: Countries without universal healthcare experience higher mortality rates.
- Rural vs. Urban Disparities: Remote areas often lack essential medical services.
- Systemic Discrimination: Ethnic minorities and low-income groups often receive inadequate medical care.
International Comparisons:
- Canada & UK: Universal healthcare models ensure broad access.
- India & South Africa: Public healthcare is available but often underfunded and overstressed.
Strategic Solutions:
- Expand insurance coverage to include marginalized communities.
- Improve telemedicine services to bridge healthcare gaps.
- Increase government investment in rural healthcare infrastructure.
5. Physical Environment: The Foundation of Health
Living conditions, air quality, and community infrastructure directly impact health outcomes.
Key Environmental Factors:
- Air and Water Quality: Pollution leads to respiratory illnesses and cancer.
- Housing Conditions: Overcrowded and poorly maintained housing increases the spread of infectious diseases.
- Urban Green Spaces: Access to parks and recreational facilities promotes physical activity and mental well-being.
Global Challenges:
- Flint Water Crisis (U.S.): Poor infrastructure led to severe lead poisoning, affecting children’s development.
- Beijing Air Pollution: Chronic air pollution contributes to high rates of lung disease.
Recommendations:
- Implement clean energy initiatives to reduce pollution.
- Design cities with green spaces and walkable areas.
- Improve water sanitation to prevent disease outbreaks.
6. Food Security and Nutrition: The Cornerstone of Public Health
Malnutrition, obesity, and food insecurity contribute to major global health concerns.
The Link Between Food and Health:
- Nutrient Deficiencies: Lead to stunted growth, cognitive impairment, and weakened immunity.
- Obesity Epidemic: Poor diet choices contribute to diabetes, heart disease, and hypertension.
- Food Deserts: Limited access to fresh produce in urban areas exacerbates health inequalities.
International Case Studies:
- Japan’s School Lunch Program: Balanced meals improve student health and academic performance.
- Brazil’s Zero Hunger Policy: Government-subsidized food programs reduce malnutrition rates.
Action Plan:
- Support local agriculture to increase food availability.
- Promote nutrition education in schools and workplaces.
- Implement subsidies for healthy foods to make nutritious choices affordable.
Conclusion: Moving Towards a Holistic Healthcare Approach
Addressing social determinants of health requires cross-sector collaboration between governments, healthcare providers, businesses, and communities. By tackling economic disparities, enhancing education, fostering social support, ensuring healthcare access, improving environmental conditions, and promoting nutritional well-being, we can create a healthier society.
Call to Action for Healthcare Leaders:
- Advocate for policy reforms that address economic and educational inequities.
- Invest in community health initiatives to support vulnerable populations.
- Promote interdisciplinary research to better understand the impact of social determinants.
By shifting our focus from reactive healthcare to proactive health promotion, we can build resilient, equitable, and thriving communities worldwide.
This revised article is structured to provide deep insights, global perspectives, and actionable solutions tailored for healthcare professionals, hospital administrators, and policymakers. It aligns with SEO best practices for ranking while maintaining an expert, engaging tone.
Here are 30 well-researched, SEO-friendly FAQs with detailed answers for your post “The Social Determinants of Health: Tackling Root Causes for a Healthier Society.” These FAQs are designed to provide valuable insights, improve search rankings, and encourage engagement.
FAQs on The Social Determinants of Health (SDOH)
Q1: What are the Social Determinants of Health (SDOH)?
A: Social Determinants of Health (SDOH) are the non-medical factors that influence health outcomes. They include economic stability, education, healthcare access, social support, environment, and public policies. These determinants shape health disparities by affecting individuals’ opportunities to live healthy lives.
Q2: Why are Social Determinants of Health important?
A: SDOH are crucial because they contribute more to overall health than medical care alone. Studies show that factors like income, education, and environment determine up to 80% of health outcomes, while healthcare services account for only 20%. Addressing SDOH helps reduce health disparities and improves population well-being.
Q3: How does income affect health outcomes?
A: Income level impacts access to healthcare, nutritious food, safe housing, and stress levels. Low-income individuals are more likely to suffer from chronic illnesses due to poor diet, inadequate medical care, and exposure to high-risk environments.
Q4: What role does education play in health?
A: Education improves health literacy, employment opportunities, and income potential. Higher education levels are linked to better access to healthcare, healthier behaviors, and longer life expectancy. Children from well-educated families are more likely to lead healthier lives.
Q5: How does housing impact health?
A: Safe, stable, and affordable housing reduces stress, prevents exposure to toxins like lead or mold, and minimizes the risk of respiratory diseases and mental health disorders. Homelessness and poor living conditions contribute to severe health issues.
Q6: How does access to healthcare affect health equity?
A: Limited healthcare access leads to untreated conditions, higher emergency room visits, and preventable deaths. Expanding healthcare coverage ensures early disease detection, vaccinations, and chronic disease management, reducing long-term health disparities.
Q7: What is the connection between employment and health?
A: Stable jobs provide financial security, access to healthcare benefits, and lower stress. Unemployment or poor working conditions contribute to anxiety, depression, and increased risk of heart disease and obesity.
Q8: How do social connections influence health?
A: Strong social networks enhance mental and physical health. Loneliness and social isolation increase the risk of heart disease, stroke, and premature death. Community support systems improve resilience and well-being.
Q9: What are food deserts, and how do they affect health?
A: Food deserts are areas with limited access to affordable, nutritious food. People living in these areas often rely on processed and unhealthy foods, increasing the risk of obesity, diabetes, and heart disease.
Q10: How does early childhood development impact lifelong health?
A: Early childhood experiences shape brain development and long-term health. Poor nutrition, lack of education, and exposure to trauma in childhood can lead to chronic diseases and mental health issues later in life.
Q11: What are the major barriers to health equity?
A: Common barriers include economic instability, racial discrimination, lack of transportation, healthcare inaccessibility, and unsafe living environments. Addressing these challenges is key to reducing health disparities.
Q12: How does environmental pollution affect health?
A: Pollution leads to respiratory diseases, cardiovascular conditions, and cancer. Poor air quality, contaminated water, and exposure to toxic chemicals disproportionately impact low-income communities.
Q13: What policies can improve Social Determinants of Health?
A: Policies supporting affordable housing, universal healthcare, quality education, and fair wages can significantly improve health outcomes and reduce inequities.
Q14: How does transportation influence health?
A: Reliable transportation improves access to healthcare, employment, and grocery stores. Lack of transportation can lead to missed medical appointments and unhealthy food choices.
Q15: What is health equity, and how does it relate to SDOH?
A: Health equity means everyone has a fair opportunity to achieve their best health. Addressing SDOH ensures resources and opportunities are distributed based on need, reducing health disparities.
Q16: What are the most vulnerable populations affected by SDOH?
A: Low-income families, minorities, the elderly, disabled individuals, and rural communities are disproportionately affected by poor social determinants of health.
Q17: Can community programs improve Social Determinants of Health?
A: Yes, community initiatives like affordable housing projects, food assistance programs, and workforce training significantly enhance health outcomes.
Q18: How do racial and ethnic disparities relate to SDOH?
A: Minority populations often face systemic barriers in education, employment, and healthcare, leading to poorer health outcomes compared to privileged groups.
Q19: What is the role of public health in addressing SDOH?
A: Public health initiatives focus on preventing diseases by improving living conditions, access to healthcare, and promoting health education.
Q20: How can businesses contribute to improving SDOH?
A: Companies can promote employee well-being by offering fair wages, healthcare benefits, and safe working conditions. Corporate social responsibility (CSR) programs also support community health initiatives.
Q21: How does gender inequality impact health?
A: Women and gender minorities often face higher healthcare costs, workplace discrimination, and domestic violence, leading to poorer health outcomes.
Q22: How does urban planning affect public health?
A: Well-designed cities with green spaces, pedestrian-friendly streets, and access to public transport encourage physical activity and reduce pollution-related illnesses.
Q23: Can digital health solutions help address SDOH?
A: Telemedicine, mobile health apps, and online health education can bridge gaps in healthcare access, especially in underserved areas.
Q24: What are examples of countries successfully addressing SDOH?
A: Countries like Sweden, Canada, and the Netherlands have strong social policies supporting universal healthcare, education, and social welfare, leading to better health outcomes.
Q25: What can individuals do to improve SDOH in their communities?
A: Volunteering, advocating for policy changes, supporting local businesses, and promoting health education can positively impact community health.
Q26: How does climate change influence social determinants of health?
A: Climate-related events like heatwaves, floods, and wildfires disproportionately affect vulnerable populations, worsening health disparities.
Q27: How do public assistance programs support SDOH?
A: Programs like Medicaid, food stamps (SNAP), and housing assistance help reduce financial stress and improve access to essential services.
Q28: What role does mental health play in SDOH?
A: Poor social conditions like poverty, discrimination, and lack of support increase the risk of depression, anxiety, and substance abuse.
Q29: How do policymakers measure the impact of SDOH interventions?
A: Metrics like life expectancy, infant mortality rates, healthcare access, and chronic disease prevalence help assess policy effectiveness.
Q30: What is the future of Social Determinants of Health?
A: With advancements in technology, data analytics, and policy reforms, future healthcare models will integrate social factors to create more equitable and effective health systems.
Want a quick walkthrough of Hospi?
We offer gentle, no-pressure demos for hospitals, labs & clinics.
Or call us directly: +91 8179508852