Looking to modernize your Hospital, Lab or Clinic?
Hospi is trusted across 25 Indian states for billing, EMR, lab reports, automations & more.
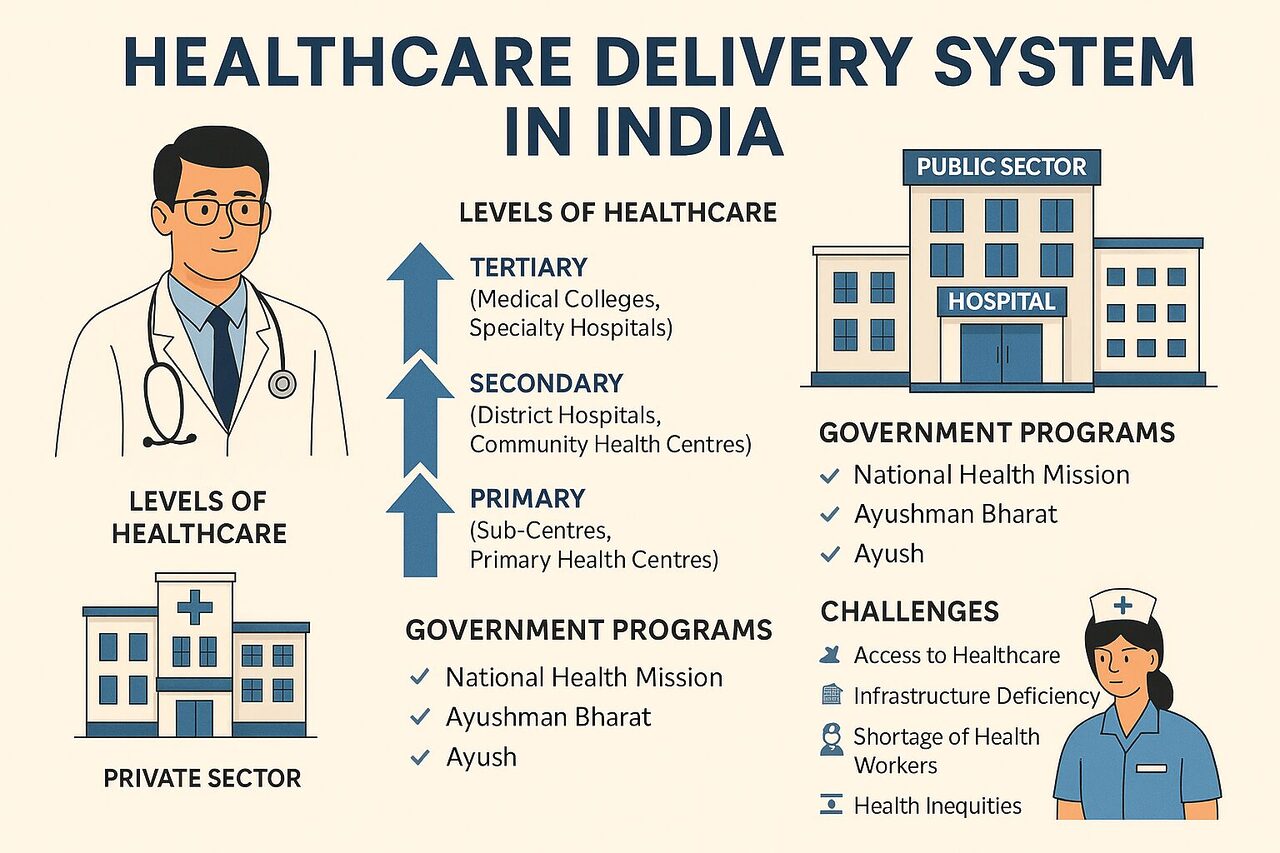
India’s healthcare delivery system is one of the largest and most complex in the world. With over 1.4 billion citizens, multiple layers of governance, and a blend of modern and traditional practices, healthcare delivery in India reflects both impressive achievements and deep-rooted challenges.
This article provides a detailed exploration of India’s healthcare delivery system—its structure, evolution, policies, institutions, challenges, and the opportunities that lie ahead.
1. Introduction: The Backbone of National Well-being
Healthcare delivery refers to the mechanism through which healthcare services are provided to individuals—ranging from preventive and promotive care to curative, rehabilitative, and palliative services.
In India, healthcare delivery is a mixed system, involving public and private providers, modern (allopathic) and traditional (AYUSH) systems, and urban as well as rural structures.
India’s Constitution guarantees health as part of the Right to Life (Article 21), placing a moral obligation on the state to ensure accessible and affordable healthcare. However, the pathway to achieving universal health coverage (UHC) remains uneven due to issues like infrastructure gaps, regional disparities, and shortage of skilled manpower.
2. Evolution of the Healthcare Delivery System in India
India’s health system has evolved significantly since independence. Here’s a brief timeline of its development:
2.1. Post-Independence Era (1947–1980)
After independence, India faced high mortality rates, infectious diseases, and poor sanitation. The Bhore Committee Report (1946) became the foundation for India’s healthcare planning, recommending:
- A three-tier healthcare structure (Primary, Secondary, Tertiary)
- Integration of preventive and curative services
- Emphasis on rural health
The government established Primary Health Centres (PHCs) and Community Health Centres (CHCs) to provide services to rural areas.
2.2. Expansion and Reforms (1980–2000)
During the 1980s and 1990s, India witnessed:
- Launch of the National Health Policy (1983)
- Introduction of immunization and family welfare programs
- Expansion of Rural Health Infrastructure under the Minimum Needs Programme
However, this period also saw an increasing role of the private sector, especially in urban and tertiary care.
2.3. The Millennium Phase (2000–2020)
With economic liberalization and globalization, healthcare became more technology-driven. Major programs included:
- National Rural Health Mission (NRHM), 2005
- National Urban Health Mission (NUHM), 2013
- Later merged as National Health Mission (NHM)
- Ayushman Bharat Program (2018) — the world’s largest publicly funded health insurance scheme
2.4. The COVID-19 Catalyst (2020 onwards)
The COVID-19 pandemic exposed vulnerabilities but also accelerated:
- Digital health adoption through the Ayushman Bharat Digital Mission (ABDM)
- Telemedicine and e-ICUs
- Focus on public health surveillance and emergency preparedness
3. Organizational Structure of Healthcare Delivery in India
India’s healthcare delivery is structured across three levels of governance and three levels of service delivery.
3.1. Administrative Framework
| Level | Governance Body | Main Responsibility |
|---|---|---|
| Central Government | Ministry of Health and Family Welfare (MoHFW) | Policy formulation, regulation, national programs |
| State Government | State Health Departments | Implementation of health programs, hospital administration |
| Local Bodies (Panchayats/Municipalities) | District & Local Health Authorities | Local level health delivery, sanitation, disease control |
The Central Government handles major programs like vaccination, disease surveillance, and research through bodies such as:
- Indian Council of Medical Research (ICMR)
- National Centre for Disease Control (NCDC)
- National Health Authority (NHA)
- AIIMS and other apex hospitals
3.2. Service Delivery Tiers
a. Primary Level (First Contact)
- Sub-Centres (SCs) — 1 per 5,000 people (rural)
- Primary Health Centres (PHCs) — 1 per 30,000 people
- Focus: Maternal-child health, immunization, minor ailments, family planning
b. Secondary Level (Referral Services)
- Community Health Centres (CHCs) — 1 per 120,000 people
- District Hospitals
- Focus: Specialist care (medicine, surgery, pediatrics, obstetrics)
c. Tertiary Level (Advanced Care)
- Medical Colleges, AIIMS, Specialty Institutes
- Focus: Super-specialized services, teaching, and research
This three-tier system ensures a referral chain from community to specialist level, though in practice, the referral mechanism often remains weak.
4. The Role of the Private Sector
India’s private healthcare sector accounts for over 70% of outpatient care and 60% of inpatient care, playing a dominant role in urban and semi-urban areas.
4.1. Key Characteristics
- Highly diverse: from small clinics to large corporate hospitals
- Major employers of doctors and nurses
- Rapid adoption of technology and quality accreditation (NABH)
- Drives medical tourism
4.2. Challenges of Private Sector Dominance
- High out-of-pocket expenditure (approx. 55% of total health spending)
- Inequality in access — affordable care remains a challenge
- Variable quality standards in unregulated facilities
To balance this, government initiatives like PM-JAY (Ayushman Bharat) have empaneled many private hospitals to provide free treatment to low-income families.
5. AYUSH: Traditional Systems of Medicine
India’s health system is uniquely pluralistic. The AYUSH department promotes:
- Ayurveda
- Yoga & Naturopathy
- Unani
- Siddha
- Homeopathy
AYUSH systems serve millions, especially in rural areas, and are integrated into PHCs and CHCs. The government encourages mainstreaming AYUSH for preventive and promotive health under National AYUSH Mission.
6. Health Financing in India
6.1. Sources of Health Financing
| Source | Share (Approx.) |
|---|---|
| Out-of-Pocket Expenditure | 55% |
| Government Spending | 30% |
| Private Insurance | 7% |
| Employer/CSR | 3% |
| External Aid & Others | 5% |
6.2. Public Health Expenditure
India spends around 2.1% of its GDP on healthcare (2023–24 data), which is low compared to developed nations (average 8–10%).
The National Health Policy 2017 targets increasing it to 2.5% of GDP by 2025.
6.3. Health Insurance Landscape
- Ayushman Bharat–PMJAY covers over 50 crore beneficiaries
- ESI, CGHS cover organized sector workers
- Private and micro-insurance schemes expanding through digital platforms
7. Human Resources in Healthcare
7.1. Manpower Status
- Doctor-population ratio: 1:834 (WHO standard: 1:1000)
- Nurse-population ratio: 1.7:1000 (needs improvement)
- Unequal distribution — most doctors are concentrated in urban areas
7.2. Skill Development Initiatives
- Skill India Mission for Healthcare
- Allied Health Professionals Bill
- Expansion of Medical Colleges & Nursing Schools
- Digital Training Platforms for ASHA and ANM workers
8. Digital Transformation in Healthcare Delivery
The future of India’s healthcare lies in digitization and data-driven decision-making.
8.1. Ayushman Bharat Digital Mission (ABDM)
Aims to create a unified digital health ecosystem with:
- Unique Health ID (ABHA Number)
- Electronic Health Records (EHRs)
- Health Facility Registry & Provider Registry
- Telemedicine integration
8.2. Telemedicine & eHealth
Platforms like eSanjeevani have enabled millions of online consultations, bridging rural-urban gaps.
AI and IoT are also being used for remote patient monitoring, predictive analytics, and disease surveillance.
9. Major National Health Programs
| Program | Objective |
|---|---|
| NHM (National Health Mission) | Universal access to equitable, affordable, quality healthcare |
| RMNCH+A | Maternal and child health |
| RNTCP (now NTEP) | Tuberculosis elimination |
| NACP | HIV/AIDS prevention and control |
| NPCDCS | Control of non-communicable diseases like diabetes, hypertension, cancer |
| National Mental Health Programme | Community-based mental healthcare |
| Ayushman Bharat PM-JAY | Free health insurance for the poor |
10. Challenges Facing India’s Healthcare Delivery System
Despite progress, several structural and functional challenges persist.
10.1. Infrastructure Gaps
- Shortage of PHCs and CHCs, especially in remote areas
- Inadequate equipment and drug availability
- Poor maintenance of public facilities
10.2. Workforce Shortages
- Uneven distribution of doctors and specialists
- Overburdened frontline workers (ASHA, ANM)
10.3. Financial Inequality
- High out-of-pocket expenditure pushes millions into poverty annually
- Insurance coverage still inadequate
10.4. Quality and Regulation
- Fragmented oversight of private healthcare
- Variability in quality and patient safety standards
10.5. Emerging Disease Burden
- Dual disease load: communicable and non-communicable diseases
- Lifestyle disorders rising in urban India
- Climate change leading to new vector-borne diseases
10.6. Data and Interoperability
- Lack of integrated data systems
- Limited use of real-time analytics in policymaking
11. Government Reforms and Innovations
11.1. Ayushman Bharat Initiative
Comprising two key pillars:
- Health and Wellness Centres (HWCs) for primary care and NCD screening
- PM-JAY for secondary and tertiary hospitalization coverage up to ₹5 lakh per family
11.2. National Digital Health Ecosystem
The ABDM connects hospitals, doctors, and patients under one digital framework—similar to India’s UPI success story in finance.
11.3. Public-Private Partnerships (PPP)
PPP models have been introduced in diagnostics, ambulance services, and teleconsultation to enhance service efficiency.
11.4. State-Level Models of Excellence
- Kerala: Strong PHC network and literacy-led awareness
- Tamil Nadu: Effective drug procurement and distribution
- Gujarat: Health insurance and private partnership models
- Telangana: Integrated digital health records and eHealth initiatives
12. Healthcare Delivery in Rural vs. Urban India
12.1. Rural Health Delivery
- 65% of population lives in rural areas
- 25,000+ PHCs and 150,000+ sub-centres operational
- Challenges: staff shortage, limited access to specialists, and poor transport
12.2. Urban Health Delivery
- Better hospital infrastructure but rising NCD burden
- Urban poor still face affordability issues
- National Urban Health Mission focuses on slum populations
13. Role of NGOs and International Agencies
NGOs and global agencies contribute to India’s healthcare ecosystem by:
- Supporting vaccination drives (UNICEF, WHO)
- Providing community health services (CARE, PATH)
- Implementing disease control programs (USAID, DFID)
- Strengthening research and innovation (Gates Foundation, ICMR partnerships)
14. Medical Tourism: A Booming Sector
India has become a global destination for affordable, high-quality medical treatment.
Key factors include:
- Skilled doctors and advanced hospitals
- Cost advantage (60–80% cheaper than Western countries)
- English-speaking medical staff
- Holistic wellness combining Ayurveda and modern medicine
Popular specialities include cardiac surgery, orthopedics, oncology, IVF, and cosmetic procedures.
In 2023, India’s medical tourism market was valued at $9 billion (≈ €8.2 billion) and is expected to reach $13 billion (≈ €11.8 billion) by 2028.
15. The Future of Healthcare Delivery in India
15.1. Vision 2047: Universal Health Coverage
India aims to ensure that every citizen receives quality healthcare without financial hardship.
Focus areas include:
- Strengthening primary care
- Expanding digital health systems
- Integrating AI and genomics
- Promoting public health education
15.2. Integration of Technology
- AI-powered diagnostics
- Blockchain for EHR security
- IoT-based health monitoring
- Predictive analytics for disease control
15.3. Preventive and Holistic Health
The future emphasizes wellness over illness—encouraging lifestyle changes, yoga, and preventive screenings.
16. Policy Recommendations
- Increase public health expenditure to at least 3% of GDP
- Strengthen PHCs and HWCs with infrastructure and staff
- Expand telemedicine and mobile health units for rural outreach
- Encourage PPP models for diagnostics and tertiary care
- Implement strict quality standards across public and private hospitals
- Focus on preventive healthcare and awareness campaigns
- Promote medical education and rural postings for young doctors
- Integrate AYUSH for community-based wellness programs
- Leverage big data for policy and disease forecasting
- Promote health equity across gender, income, and geography
17. Conclusion
The healthcare delivery system in India is a living example of resilience, diversity, and reform. Despite challenges like infrastructure gaps and inequities, India has made tremendous progress—from eliminating polio to launching the world’s largest digital health initiative.
The road ahead lies in strengthening primary care, leveraging technology, and ensuring equitable access for all citizens.
As India moves toward its 100th year of independence in 2047, a strong, inclusive, and digital healthcare delivery system will be central to its vision of a “Healthy Bharat.”
Top 50 FAQs on the Healthcare Delivery System in India
1. What is the healthcare delivery system in India?
The healthcare delivery system in India refers to the organized framework through which healthcare services are provided to citizens. It includes public and private providers, modern medicine (allopathy) and traditional systems (AYUSH), and operates at three levels — primary, secondary, and tertiary care.
2. What are the main components of India’s healthcare delivery system?
The main components include:
- Primary Health Centres (PHCs) and Sub-Centres for basic care
- Community Health Centres (CHCs) and District Hospitals for specialized care
- Medical Colleges and AIIMS for advanced and tertiary care
- Private hospitals, clinics, and diagnostic centres for additional capacity
3. How is healthcare structured in India?
India follows a three-tier structure:
- Primary level – basic care through PHCs and Sub-Centres
- Secondary level – referral care at CHCs and District Hospitals
- Tertiary level – specialized and super-specialized services at teaching hospitals and research institutes
4. Who governs healthcare delivery in India?
Healthcare in India is a State subject, but responsibilities are shared between the Central Government and State Governments.
- The Ministry of Health and Family Welfare (MoHFW) oversees national policies.
- State Health Departments manage hospitals, manpower, and local implementation.
5. What is the role of the Ministry of Health and Family Welfare (MoHFW)?
The MoHFW formulates national health policies, regulates healthcare institutions, implements national programs like NHM and Ayushman Bharat, and coordinates between states and central agencies for public health improvement.
6. What are the three levels of healthcare in India?
- Primary Care: Preventive and basic curative care through PHCs.
- Secondary Care: Specialist care at CHCs and district hospitals.
- Tertiary Care: Advanced diagnostic, surgical, and super-specialty services at medical colleges and apex institutes.
7. What is a Primary Health Centre (PHC)?
A PHC serves as the first contact point between community and health services. Each PHC covers about 30,000 people and provides maternal-child care, immunization, family planning, and treatment of minor illnesses.
8. What is a Community Health Centre (CHC)?
A CHC serves as a referral unit for four PHCs and caters to about 1,20,000 people. It provides specialist services in medicine, surgery, pediatrics, and obstetrics/gynecology.
9. What is the National Health Mission (NHM)?
Launched in 2013 by merging the NRHM and NUHM, the National Health Mission aims to provide equitable, affordable, and quality healthcare with a focus on strengthening rural and urban public health infrastructure.
10. What is Ayushman Bharat?
Ayushman Bharat is a flagship initiative launched in 2018, with two key components:
- Health and Wellness Centres (HWCs) for primary care
- PM-JAY (Pradhan Mantri Jan Arogya Yojana) — free health insurance coverage of ₹5 lakh per family per year for secondary and tertiary care
11. What is the Ayushman Bharat Digital Mission (ABDM)?
ABDM aims to create a digital health ecosystem by providing every citizen with a unique Health ID (ABHA Number) and enabling electronic health records accessible across hospitals and doctors nationwide.
12. What is the role of private hospitals in India’s healthcare system?
Private hospitals provide over 70% of outpatient and 60% of inpatient care in India. They are vital in tertiary care, diagnostics, and specialized treatments, but their services are often more expensive than public options.
13. What are the key challenges of India’s healthcare system?
Major challenges include:
- Inadequate infrastructure
- Shortage of skilled workforce
- High out-of-pocket expenses
- Unequal access between rural and urban areas
- Weak referral and data systems
14. What is the ratio of doctors to population in India?
India’s doctor-to-population ratio is approximately 1:834, which meets the WHO’s minimum standard of 1:1000, but distribution remains uneven — most doctors work in urban regions.
15. How much does India spend on healthcare?
As of 2024, India’s public health expenditure is around 2.1% of GDP. The National Health Policy 2017 aims to raise this to 2.5% of GDP by 2025.
16. What are Health and Wellness Centres (HWCs)?
HWCs are upgraded PHCs or Sub-Centres offering comprehensive primary healthcare, including NCD screening, mental health, elderly care, and telemedicine services under the Ayushman Bharat scheme.
17. What is the role of ASHA workers in India?
ASHA (Accredited Social Health Activist) workers act as community link workers, promoting health awareness, maternal-child care, immunization, and facilitating access to public health programs in villages.
18. What is AYUSH in India?
AYUSH stands for Ayurveda, Yoga & Naturopathy, Unani, Siddha, and Homeopathy. It represents India’s traditional systems of medicine, integrated with the national health policy for holistic healthcare.
19. How does India’s healthcare compare to developed countries?
India has made significant progress in life expectancy and disease control but still lags in public health spending, doctor density, and quality of rural services compared to countries like the UK or Japan.
20. What is Universal Health Coverage (UHC)?
UHC means ensuring all people have access to quality health services without financial hardship. India is progressing toward UHC through Ayushman Bharat and digital health initiatives.
21. What is the role of the Indian Council of Medical Research (ICMR)?
ICMR leads medical research, disease surveillance, and vaccine development. It played a vital role during the COVID-19 pandemic and continues to guide India’s health research agenda.
22. What are the key national health programs in India?
Major programs include:
- National Health Mission (NHM)
- National TB Elimination Programme (NTEP)
- National AIDS Control Programme (NACP)
- National Mental Health Programme (NMHP)
- NPCDCS for non-communicable diseases
23. What is PM-JAY and who benefits from it?
Pradhan Mantri Jan Arogya Yojana (PM-JAY) provides free hospitalization coverage of up to ₹5 lakh per year to over 10 crore poor and vulnerable families, covering more than 50 crore citizens.
24. What are the roles of District Hospitals?
District hospitals are secondary-level healthcare institutions that provide specialist services and act as referral centres for CHCs. They handle surgery, emergency, obstetrics, and diagnostics.
25. How is health financed in India?
India’s health financing comes from:
- Government spending (≈30%)
- Out-of-pocket payments (≈55%)
- Private insurance (≈7%)
- Social security and employer funds (≈8%)
26. Why is out-of-pocket expenditure high in India?
Because public healthcare coverage is limited and private hospitals dominate urban healthcare, patients often pay directly for medicines, diagnostics, and treatment, raising financial burdens.
27. What is telemedicine in India?
Telemedicine allows patients to consult doctors remotely via video or phone. The government’s eSanjeevani platform has facilitated over 20 crore consultations since 2020.
28. How has COVID-19 changed India’s healthcare delivery?
COVID-19 accelerated:
- Digital health adoption
- Investment in public health infrastructure
- Vaccine manufacturing
- Emergency preparedness and surveillance mechanisms
29. What is the role of technology in India’s healthcare system?
Technology drives improvements through:
- Digital Health IDs
- Telemedicine and e-Hospitals
- AI-based diagnostics
- IoT-enabled monitoring
- Blockchain in EHR management
30. What is the role of NGOs in healthcare delivery?
NGOs like CARE India, PATH, and SEWA support public health programs, vaccination drives, and maternal-child care. They act as partners in community outreach and disease control.
31. What is the role of local governments in healthcare?
Local bodies like Panchayats and Municipalities manage sanitation, water supply, local clinics, and immunization programs under the guidance of district health authorities.
32. What are the major diseases targeted by India’s health programs?
India focuses on controlling tuberculosis, malaria, HIV/AIDS, leprosy, cancer, diabetes, and hypertension, along with maternal and child mortality reduction.
33. What are some successful state models in healthcare?
- Kerala: Strong PHC system and literacy-led awareness
- Tamil Nadu: Efficient drug procurement and distribution
- Gujarat: Health insurance integration
- Telangana: Digital health records and telemedicine adoption
34. What are the benefits of the Ayushman Bharat scheme?
- Free hospitalization up to ₹5 lakh per year
- No restriction on family size or age
- Cashless treatment in empaneled hospitals
- Coverage of pre-existing diseases
- Availability across public and private hospitals
35. How does India ensure medicine availability in public hospitals?
Many states, such as Tamil Nadu and Rajasthan, have centralized drug procurement systems ensuring availability of essential medicines free of cost in government hospitals.
36. What is the role of AIIMS in India’s health system?
The All India Institute of Medical Sciences (AIIMS) serves as a centre of excellence in tertiary care, medical education, and research. It also acts as a model for other teaching hospitals.
37. What is the current focus of India’s National Health Policy 2017?
The policy emphasizes:
- Universal health coverage
- Digital health
- Strengthening PHCs
- Preventive care
- Increasing public health spending to 2.5% of GDP
38. What is India’s doctor-nurse ratio?
India has roughly 1.7 nurses per 1,000 people, below the WHO norm of 3 per 1,000. The government is expanding nursing colleges and paramedical training to bridge this gap.
39. How does India manage non-communicable diseases (NCDs)?
Through the NPCDCS program, India promotes early screening, lifestyle modification, and treatment for diseases like diabetes, hypertension, and cancer at HWCs and CHCs.
40. What is medical tourism in India?
India attracts global patients seeking affordable, high-quality treatment in areas like cardiac surgery, orthopedics, IVF, and oncology. The sector was worth $9 billion in 2023 (€8.2 billion) and continues to grow.
41. How do rural and urban healthcare systems differ in India?
Rural areas depend heavily on PHCs and ASHA workers, facing infrastructure and staff shortages. Urban areas have advanced hospitals but high treatment costs, creating affordability gaps.
42. What is the role of digital health IDs?
Digital Health IDs (ABHA Numbers) enable secure storage and sharing of patients’ medical records, improving coordination and continuity of care across hospitals and doctors.
43. How is mental healthcare addressed in India?
Under the National Mental Health Programme (NMHP), India promotes community-based mental health services, awareness, and free psychiatric medicines at district hospitals.
44. What are the achievements of India’s healthcare system?
- Eradication of polio
- Reduction in maternal and infant mortality
- Large-scale vaccination success
- World’s largest public health insurance (PM-JAY)
- Rapid digital transformation (ABDM)
45. What are the goals of “Healthy India 2047”?
By 2047, India aims to:
- Achieve Universal Health Coverage
- Strengthen PHCs and digital health
- Integrate traditional and modern medicine
- Reduce disease burden and health inequities
46. How are healthcare professionals trained in India?
India has over 700 medical colleges and 3,000 nursing schools regulated by NMC (National Medical Commission) and INC (Indian Nursing Council) to ensure quality education and skill development.
47. What is the future of digital healthcare in India?
The future includes AI-powered diagnostics, wearable health trackers, predictive analytics, and nationwide interoperability through ABDM, creating a fully connected digital health ecosystem.
48. How is India addressing health inequity?
Through targeted schemes like PM-JAY, rural health missions, tribal outreach programs, and free drug distribution, India aims to ensure equitable healthcare access across socio-economic groups.
49. What is the role of data in improving healthcare delivery?
Health data enables disease surveillance, policy planning, and early detection of outbreaks. The integration of ABDM will allow real-time data analysis for informed decision-making.
50. What is the way forward for India’s healthcare system?
India’s path forward lies in:
- Strengthening primary healthcare
- Expanding public health investment
- Leveraging technology and AI
- Integrating preventive and holistic care
- Building a resilient, inclusive, and digital-first healthcare ecosystem
Want a quick walkthrough of Hospi?
We offer gentle, no-pressure demos for hospitals, labs & clinics.
Or call us directly: +91 8179508852