Looking to modernize your Hospital, Lab or Clinic?
Hospi is trusted across 25 Indian states for billing, EMR, lab reports, automations & more.
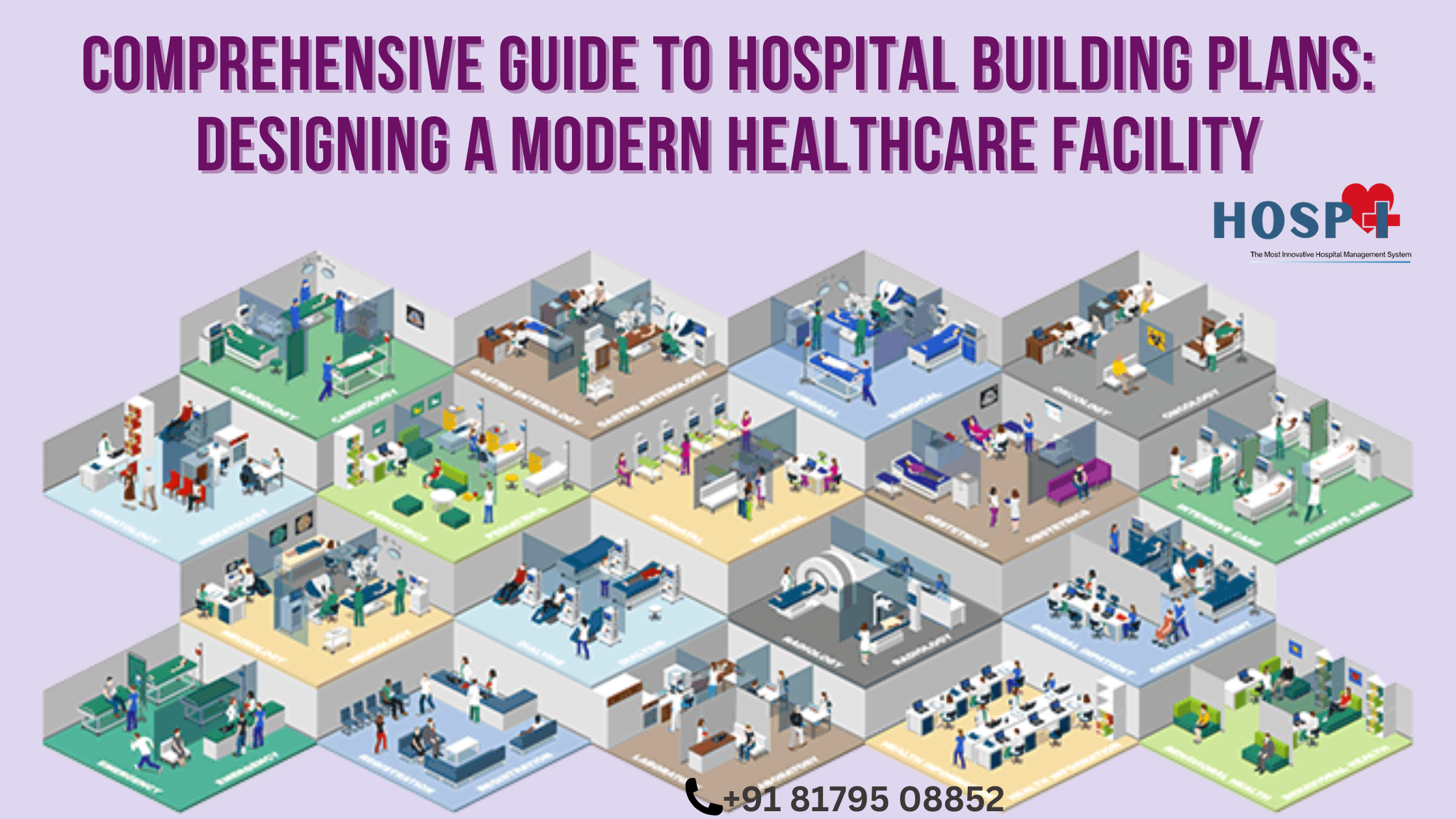
Designing a modern hospital is one of the most challenging infrastructure projects in the world. A hospital is not just a building—it is a lifesaving ecosystem that must support medical excellence, patient experience, infection control, technology, resilience, and cost-efficiency for decades.
While the principles of hospital planning are universal, the costs, standards, regulatory frameworks, patient loads, climate considerations, and design preferences vary significantly across countries.
This global guide explores how hospitals are planned in regions like the United States, United Kingdom, Russia, China, India, Africa, Europe, and the Middle East, giving you international benchmarks, numbers, and comparison tables to help plan a future-ready hospital anywhere in the world.
1. Why Modern Hospital Planning Must Adopt a Global View
Healthcare needs are changing rapidly across the planet:
- The US demands technologically advanced, highly regulated facilities.
- The UK emphasizes NHS compliance, fire safety, and patient dignity.
- Russia focuses on centralized care and high resilience to extreme climates.
- China prioritizes speed, scale, and infection-control–driven design.
- India balances affordability, scalability, and high patient volumes.
- Africa focuses on accessibility, sustainability, and essential services.
- GCC countries invest heavily in luxury healthcare and ultramodern facilities.
Understanding these differences helps architects, hospital owners, healthcare investors, and policymakers develop globally competitive, efficient hospitals.
2. Core Principles of Hospital Building Planning (Applicable Worldwide)
Regardless of country, every modern hospital must follow six foundational principles:
2.1 Patient Safety
- Clean–dirty separation
- Infection control zoning
- Emergency access
- Disaster resilience
2.2 Operational Efficiency
- Logical department adjacency
- Optimized staff movement
- Automated workflows
2.3 Patient Experience
- Noise control
- Privacy standards
- Easy navigation
- Natural light & biophilic elements
2.4 Scalability
- Modular expansions
- Vertical & horizontal growth options
- Future-readiness for technology
2.5 Sustainability
- Energy efficiency
- Water recycling
- Solar or hybrid power systems
2.6 Digital Integration
- Telemedicine
- HIS/LIS/RIS/PACS
- Smart building systems
3. International Comparison: Hospital Planning Standards by Country
Below is a high-level comparison of hospital planning characteristics.
Table 1: Differences in Hospital Planning Approach Across Countries
| Region | Average Bed Size in New Hospitals | Planning Priority | Cost per Bed (USD) | Digital Adoption | Expansion Focus |
|---|---|---|---|---|---|
| USA | 150–400 | Technology, safety, regulations | $1M–$3M | Very High | Moderate |
| UK | 200–600 (NHS) | Patient dignity, fire safety | $900k–$2M | High | High |
| Russia | 250–800 | Disaster resilience, central hubs | $700k–$1.6M | Medium | Low |
| China | 500–1500 | Speed, scalability, mass capacity | $500k–$1.2M | High | Very High |
| India | 100–400 | Affordability, patient flow | $200k–$600k | Medium | Very High |
| Africa | 50–250 | Accessibility, sustainability | $150k–$400k | Low–Medium | Medium |
| GCC | 100–300 | Luxury, smart hospitals | $800k–$2.5M | Very High | High |
| Europe (EU) | 150–350 | Safety, energy efficiency | $1M–$2.2M | High | Moderate |
4. Global Cost Comparison for Building Hospitals
Costs vary widely based on land prices, labor, medical equipment, and local regulations.
Table 2: Cost Comparison (Land, Civil, MEP, Equipment)
| Region | Cost per sq.ft (USD) | Cost per Bed (USD) | Cost per Bed (EUR) |
|---|---|---|---|
| USA | $600–$1200 | $1M–$3M | €920k–€2.75M |
| UK | $450–$1100 | $900k–$2M | €825k–€1.83M |
| EU (General) | $400–$1000 | $1M–$2.2M | €915k–€2M |
| China | $150–$450 | $500k–$1.2M | €460k–€1.1M |
| Russia | $200–$600 | $700k–$1.6M | €640k–€1.46M |
| India | $80–$200 | $200k–$600k | €185k–€550k |
| Africa | $50–$180 | $150k–$400k | €140k–€370k |
| Middle East (GCC) | $300–$900 | $800k–$2.5M | €730k–€2.3M |
5. Detailed Department-Wise Planning with International Considerations
5.1 Emergency Department (ED)
Global differences
- US: Trauma Level 1/2 compliant, segregated ambulance bays.
- UK: NHS Accident & Emergency (A&E) guidelines.
- Russia: Large triage centers attached to polyclinics.
- China: Very high patient volume design.
- India/Africa: Flexible trauma + general emergency due to mixed cases.
Ideal features:
- 2 separate entrances (walk-in & ambulance).
- Resuscitation bays: 200–300 sq.ft each.
- Isolation zone for infectious diseases.
5.2 Outpatient Department (OPD)
Key international differences
- US/UK/EU: Larger rooms (120–160 sq.ft).
- India/Africa: High volume OPDs; 60–90 sq.ft rooms common.
- China: Ultra-high waiting capacities (500–1500 people).
Best practices:
- Queue management systems
- Self-registration kiosks
- Cluster-based specialty planning
- Separate diagnostic corridor
5.3 ICU Planning Across Regions
Comparison Table
| Region | ICU Beds as % of Total | Bed Space (sq.ft) | Key Feature |
|---|---|---|---|
| US | 10–20% | 250–300 | High technology dependency |
| UK | 8–15% | 200–260 | NHS HTM compliant airflow |
| Russia | 10–18% | 210–270 | High isolation capability |
| China | 5–12% | 180–230 | Large ICU halls common |
| India | 5–10% | 150–200 | Mixed ICU/HDU concept |
| Africa | 3–8% | 120–150 | Basic critical units |
5.4 Operating Theatres (OTs)
International OT Sizes:
- US/UK/EU: 600–800 sq.ft
- China: 500–650 sq.ft
- Russia: 550–700 sq.ft
- India/Africa: 400–550 sq.ft
Must-haves worldwide:
- HEPA filters
- Laminar airflow
- Hermetic doors
- Scrub area outside each OT
- Separate sterile & dirty corridors
5.5 Radiology Department
Global differences:
- US/EU: Strict radiation shielding regulations.
- India/Africa: AERB / ARPB compliance (lighter but adequate).
- China: Speed of installation prioritized.
Equipment Clearances:
- CT Room: 240–300 sq.ft
- MRI Room: 400–450 sq.ft + RF shielding
5.6 Wards & Patient Rooms
Global Comparison Table
| Country/Region | Single Room Size | Twin Room Size | Isolation Room |
|---|---|---|---|
| US | 150–200 sq.ft | 220–280 sq.ft | Negative pressure mandatory |
| UK | 140–180 sq.ft | 220–260 sq.ft | NHS HTM standards |
| EU | 150–190 sq.ft | 210–250 sq.ft | EU Health Safety norms |
| China | 120–160 sq.ft | 180–240 sq.ft | Moderate standards |
| Russia | 130–170 sq.ft | 190–250 sq.ft | High winter insulation |
| India | 90–140 sq.ft | 150–200 sq.ft | Isolation optional |
| Africa | 80–120 sq.ft | 140–180 sq.ft | Often shared wards |
6. Global Zoning Principles
Almost all countries follow a variation of the same zoning model:
6.1 Critical Zone
ICU, OT, CSSD, Cath Lab
6.2 Semi-Critical Zone
Diagnostics, daycare, minor procedures
6.3 Non-Critical Zone
OPD, pharmacy, administration
6.4 Support Zone
Kitchen, laundry, engineering
6.5 Public vs. Staff Zoning
Separate lifts, corridors, and entries worldwide.
But differences exist:
- US/UK/EU: Strict segregation mandated.
- India/Africa: Segregation exists but often flexible.
- China: Separate flows designed for pandemics.
7. Engineering Systems: International Differences
7.1 HVAC Standards
| Region | Fresh Air Requirement | Filtration | Temperature |
|---|---|---|---|
| US (ASHRAE) | 15–20% | HEPA 0.3μ | 20–24°C |
| UK NHS HTM | 10–15% | HEPA | 19–23°C |
| EU | 12–18% | HEPA | 20–24°C |
| China | 10–15% | Moderate | 20–26°C |
| India | 8–15% | Varies | 22–28°C |
| Africa | 5–12% | Basic | 23–30°C |
7.2 Electrical & Backup Systems
- US/EU: Dual-feed + N+1 redundancy
- India/China: DG backup + UPS
- Africa: Hybrid solar + diesel
- GCC: Central command center + automation
7.3 Medical Gas Pipeline Systems (MGPS)
Standardized worldwide:
- Oxygen
- Vacuum
- Compressed air
- Nitrous oxide
But installation quality varies by region due to certification norms.
8. Infection Control Planning Across Countries
Countries with strictest standards:
- US (CDC guidelines)
- UK (NHS IPC)
- Germany & France
- Japan
Countries with fast-evolving standards:
- China (after COVID-19)
- India
- Middle East
- Africa
Key infection-control design elements:
- Negative pressure rooms
- Separate dirty corridors
- Touchless design
- UV sterilization integration
- Handwashing stations at every entry
9. Sustainability Requirements Globally
US/EU/UK
- LEED or BREEAM certification
- High energy efficiency
- Solar + geothermal common
India
- GRIHA certification
- Solar power & rainwater harvesting mandatory in many states
China
- Green building codes
- District cooling/heating
Africa
- Solar-first strategy
- Water recycling critical
10. Bed-Wise Planning Differences Across Countries
Table 3: Typical Bed Strength & Land Requirement
| Size | US/UK/EU Land | China Land | India Land | Africa Land |
|---|---|---|---|---|
| 50-bed | 2–3 acres | 1.5–2 acres | 1–1.5 acres | 1–2 acres |
| 100-bed | 4–6 acres | 3–4 acres | 2–3 acres | 2–4 acres |
| 200-bed | 8–12 acres | 6–8 acres | 4–5 acres | 3–6 acres |
| 500-bed | 20–30 acres | 10–15 acres | 8–12 acres | 6–10 acres |
11. Legal and Regulatory Standards by Country
US
- Joint Commission (JCI)
- NFPA
- ASHRAE
- OSHA
UK
- NHS Health Technical Memoranda (HTM)
- Care Quality Commission (CQC)
EU
- EN standards
- Local health authority regulations
Russia
- SanPiN norms
China
- National Health Construction Code
India
- NABH, AERB, Fire NOC
Africa
- Government health standards
- Often WHO-based frameworks
12. Future Trends in Global Hospital Design
Smart Hospitals
US, GCC, Singapore leading adoption.
Modular Construction
China: Built 1,000-bed hospitals in 10 days during COVID.
Telemedicine-Compatible Architecture
India, Africa, and Europe rapidly expanding.
Hybrid Operating Theatres
Becoming standard across US, UK, EU, China, Middle East.
AI-Powered Flow Management
Used heavily in large US/Chinese hospitals.
13. Common Mistakes in Hospital Planning (Worldwide)
- Wrong adjacency planning
- Underestimating outpatient volumes
- Poor emergency access
- Under-provisioning parking
- Inadequate vertical expansion plans
- Insufficient HVAC tonnage
- Failure to plan for pandemics
- Ignoring cultural needs (e.g., family space in India/China/Africa)
14. Conclusion
Designing a global-standard hospital requires a deep understanding of architecture, engineering, clinical needs, regulations, patient psychology, digital transformation, and future scalability.
The best hospital plans combine:
- US-level technology
- UK-level safety
- EU-level sustainability
- China-level scalability
- India-level efficiency
- Africa-level accessibility
- GCC-level smart innovation
With thoughtful planning, your healthcare facility can be future-ready, globally compliant, financially viable, and truly patient-centered.
50 FAQs on Hospital Building Plans
1. What is a hospital building plan?
A hospital building plan is a detailed architectural and engineering blueprint that outlines the layout, zoning, departments, utilities, patient pathways, emergency areas, infection-control features, and technical systems needed to construct a modern healthcare facility.
2. Why is hospital planning different from regular building planning?
Hospitals require specialized areas such as ICUs, operation theatres, labs, radiology, emergency zones, medical gas systems, waste management, and strict infection control—all of which demand far more complexity than commercial or residential buildings.
3. How many acres of land are required for a 100-bed hospital?
Land requirements vary by region:
- US/UK/EU: 4–6 acres
- China: 3–4 acres
- India: 2–3 acres
- Africa: 2–4 acres
4. What is the average cost to build a hospital?
Costs differ globally:
- USA: $1M–$3M per bed
- Europe: $1M–$2.2M per bed
- China: $500k–$1.2M per bed
- India: $200k–$600k per bed
- Africa: $150k–$400k per bed
5. What departments are mandatory in a multispecialty hospital?
Typically required departments include OPD, Emergency, ICU, OTs, Radiology, Laboratory, Pharmacy, Wards, CSSD, Administrative block, Kitchen, Laundry, and Engineering services.
6. What is zoning in hospital design?
Zoning divides the hospital into critical, semi-critical, non-critical, and support areas to ensure infection control, smooth patient flow, and operational efficiency.
7. Why is adjacency planning important?
Correct adjacency reduces staff fatigue, speeds up diagnosis, minimizes patient movement, and improves emergency response time.
8. How are hospitals planned for pandemics?
Modern hospital plans include isolation rooms, negative pressure wards, separate infectious patient entries, donning/doffing rooms, and flexible conversion spaces.
9. What is the ideal size of an ICU room?
The average global size:
- US/UK/EU: 250–300 sq.ft
- India/China: 150–200 sq.ft
- Africa: 120–150 sq.ft
10. How many operation theatres should a 100-bed hospital have?
Typically 4–6 OTs, depending on specialties and patient volume.
11. What HVAC standards do hospitals follow worldwide?
Countries follow ASHRAE (US), HTM (UK), EN standards (EU), NABH (India), MOH (China), and national guidelines to ensure proper air pressure and filtration.
12. What is the difference between a negative and positive pressure room?
- Negative pressure: Prevents infectious air from escaping (TB, COVID).
- Positive pressure: Keeps contaminated air from entering (OTs, transplant rooms).
13. How do countries differ in emergency department design?
US and UK follow strict trauma-level standards; China and India design for heavy footfall; Africa focuses on essential emergency care with basic triage.
14. What is the role of medical gas pipelines (MGPS)?
MGPS supplies oxygen, compressed air, nitrous oxide, and vacuum across clinical areas with alarms and redundancy.
15. Why is natural light important in hospital design?
It improves mood, speeds recovery, reduces patient stress, lowers energy costs, and enhances overall patient experience.
16. What is the lifespan of a hospital building?
Most modern hospitals are designed for 50–75 years of operational life with periodic renovations.
17. How do building codes differ by country?
The US uses NFPA and IBC codes; UK uses HTM/HBN; EU follows EN standards; India uses NBC; Africa often follows WHO guidance plus local regulation.
18. What is a hybrid operating theatre?
A hybrid OT combines high-end imaging (CT, MRI, Cath Lab) inside an OT to enable complex surgeries and minimally invasive procedures.
19. What sustainability features should hospitals include?
Solar power, rainwater harvesting, LED lighting, BMS automation, efficient HVAC, green roofs, and wastewater recycling.
20. Why are separate corridors needed for patients and staff?
It reduces infection risk, prevents overcrowding, improves workflow, and enhances privacy.
21. What is functional space programming?
It defines room sizes, equipment layout, spatial relationships, and utilities for every department.
22. How long does it take to build a hospital?
Timelines vary:
- China: 6–24 months
- India/Africa: 18–36 months
- US/EU/UK: 3–5 years (due to regulations and inspections)
23. What is the ideal bed-to-toilet ratio?
Globally acceptable ratio: 1 toilet for every 4–6 beds, but premium hospitals often provide 1 toilet per bed.
24. Are modular hospitals becoming popular?
Yes. Modular construction reduces cost, speeds up completion, and allows scalability—widely used in China, Middle East, and Europe.
25. Why is the location of a hospital critical?
Key factors: accessibility, population density, road connectivity, emergency access, land availability, and proximity to other healthcare facilities.
26. How important is flood or earthquake resistance?
Essential. US, Japan, Turkey, and Indonesia follow strict seismic codes. Flood-resistant design is crucial in India, Bangladesh, and African nations.
27. What are smart hospitals?
Hospitals using IoT, AI, automated workflows, digital patient records, real-time tracking, telemedicine, and integrated nurse call systems.
28. What is CSSD and why is it critical?
CSSD (Central Sterile Supply Department) handles cleaning, sterilizing, and storing surgical instruments to ensure infection-free surgical operations.
29. Why do hospitals need separate lifts for patients and materials?
To prevent cross-contamination and ensure smooth logistics (food, laundry, waste, supplies).
30. What is the typical ROI period for a new hospital?
ROI usually ranges from 5 to 12 years, depending on country, specialty mix, and operational efficiency.
31. Why is workflow mapping done?
It analyzes patient, staff, and material movement to avoid bottlenecks and optimize productivity.
32. How many OPD rooms are needed in a 100-bed hospital?
Typically 20–30 consultation rooms, depending on specialties.
33. What is the role of BIM in hospital design?
BIM (Building Information Modeling) helps visualize the entire hospital, prevent clashes, optimize engineering systems, and reduce construction errors.
34. Why are fire exits and sprinklers mandatory?
To ensure safe evacuation and minimize damage—mandatory in almost all global building codes.
35. What IT systems are essential in modern hospitals?
HIS, EMR, PACS, LIS, RIS, telemedicine, queue management, and CCTV monitoring.
36. What is a nurse station and why is it centrally located?
It’s the clinical operations hub on each floor, enabling fast monitoring and response to patient needs.
37. Do all hospitals require MRI and CT?
Not necessarily. Small hospitals may outsource advanced radiology, while large hospitals and tertiary centers have in-house CT, MRI, PET-CT.
38. What is the average construction cost of a 200-bed hospital?
Globally:
- USA/EU: $200M–$400M
- China: $80M–$180M
- India: $40M–$120M
- Africa: $25M–$80M
39. Why is ventilation critical in hospitals?
Proper ventilation reduces infection risk, prevents airborne transmission, and maintains clinical air quality.
40. What are the most common design mistakes in hospitals?
Poor zoning, lack of future expansion space, insufficient parking, inadequate HVAC, and wrong department adjacency.
41. What is a patient-centered hospital design?
A design that focuses on comfort, natural light, privacy, noise control, easy navigation, and family-friendly spaces.
42. How many elevators should a mid-size hospital have?
At least 5–8 elevators including patient lifts, staff lifts, and service lifts.
43. Why do hospitals require separate waste management systems?
To safely handle biomedical, infectious, chemical, and general waste as per global regulations.
44. What is the typical area required per hospital bed?
Globally accepted range: 800–1200 sq.ft per bed, including common spaces and utilities.
45. Why is parking important in hospital planning?
To accommodate patients, attendants, staff, ambulances, and supply vehicles—average requirement: 1 parking per 3 beds.
46. How often should hospitals be renovated?
Minor renovations every 5–7 years, major upgrades every 15–20 years.
47. What climate considerations affect hospital design?
- Cold countries need thermal insulation and humidity control.
- Hot countries require enhanced HVAC and sun-shading.
- Tropical regions need strong mold and moisture control.
48. What are universal design standards in hospitals?
Ramps, wide corridors, anti-skid flooring, braille signage, wheelchair-friendly washrooms, and accessibility lifts.
49. Why do hospitals use antibacterial materials?
To reduce infection risk—materials include epoxy flooring, antimicrobial wall panels, and copper alloy touchpoints.
50. What future technologies will shape hospital buildings?
AI monitoring, robotic pharmacies, drone drug delivery, digital twins, AR-assisted surgery, and fully automated smart wards.
Want a quick walkthrough of Hospi?
We offer gentle, no-pressure demos for hospitals, labs & clinics.
Or call us directly: +91 8179508852